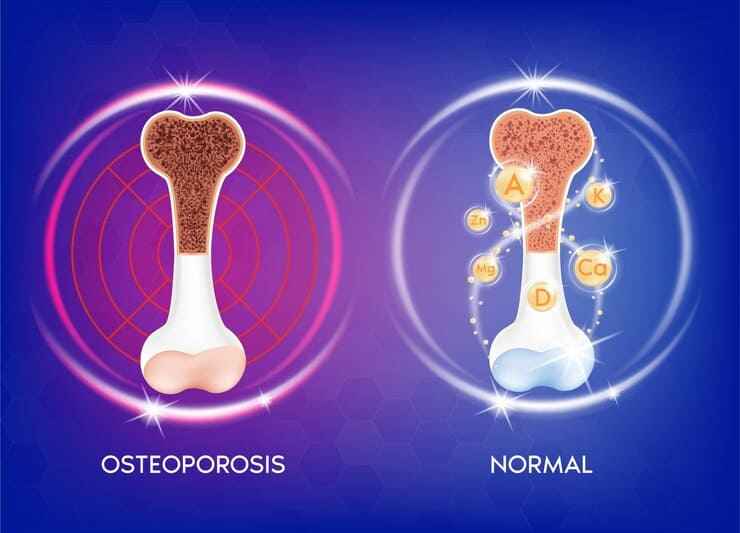
Osteoporosis is a condition in which bones become weak and brittle, raising the risk of fractures. After menopause, women are more likely to develop postmenopausal osteoporosis. When a woman approaches menopause, her levels of the sex hormones drop, and eventually, periods stop. These hormones have an impact on bone development as well, and therefore, lower levels may result in reduced bone density. Osteoporosis, which is a common problem in postmenopausal women, is due to decreased bones mineral density.
Lower estrogen and progesterone levels have been linked to postmenopausal osteoporosis. Estrogen hormone affects specific bone cells called osteoclasts, osteoblasts, and osteocytes, as well as hormone synthesis. Women who have reached menopause do not realize that they have osteoporosis until they have broken bone.
Symptoms
Fractures caused by osteoporosis most usually damage the hip, vertebrae, or wrist. Additional bones, like those in the arm or pelvis, can also be broken. A fracture can occasionally be caused by anything as simple as coughing or sneezing and also by physical activity that puts additional pressure on the bones.
Other symptoms associated with menopause, in addition to weak and brittle bones, include the following:
- Hot flashes
- Vaginal dryness
- Headaches
- Anxiety
- Mood changes
- Night sweats
- Diminished sex drive
- Swollen joints
- Joint stiffness
- Palpitations
Relationship between menopause and osteoporosis
The absence of estrogen in perimenopause and menopause is linked to the development of osteoporosis. Early menopause (before the age of 45) and any extended perimenopausal period when estrogen levels are low and menstrual cycles are missing or rare or absent – can lead to postmenopausal osteoporosis.
Causes of postmenopausal Osteoporosis
Menopause accelerates bone loss, increasing the risk of osteoporosis. Bones are made up of a series of proteins and minerals that give them the strength and mobility to support the body’s movement. They also contain special cells like osteocytes that aid in the maintenance of the network of bone cells. The hormone estrogen is one such factor that can impact bone structure.
Although scientists aren’t sure how estrogen makes bones healthy, they believe osteocytes produce a protein called SEMA3A that preserves the bone matrix in good shape. They say that as individuals age, their estrogen and SEMA3A levels decline, and osteocytes die, causing bones to lose their structural integrity.
Diagnosis (screening)
A bone mass scan, also known as a DEXA scan, may be performed if a doctor suspects osteoporosis. This scan is quick and painless, taking about 10–20 minutes to complete. The patient lies on their back on an X-ray table for the scanning process.
The test results are then analyzed by a doctor to assess the woman’s bone density. Your doctor usually calculates and evaluates the results based on a young adult’s bone density and determines the difference as a standard deviation (SD). The result of this calculation is a T score. A T score of more than -1 SD is considered normal, whereas a value of -1 to -2.5 indicates considerable bone loss (osteopenia), and a score of -2.5 or less indicates osteoporosis.
Treatment
Selective estrogen receptor modulators (SERMS) – These medicines mimic estrogen and hence help in preventing osteoporosis.
Bisphosphonates may be prescribed to slow down bone loss.
Hormone Replacement Therapy (HRT) – gynecologists sometimes recommend this treatment to address menopause. However, this treatment is not specifically recommended to address osteoporosis.
Calcium and vitamin D supplements: Both these supplements help in improving bones’ mineral density and strength.
Bottom line
Osteoporosis caused by reduced estrogen levels is known as postmenopausal osteoporosis. As there are no other symptoms or indicators of osteoporosis besides fractures, risk assessment is required to detect those who are at a higher risk of bone loss and osteoporosis. A bone density scan may be used by a gynecologist to help detect postmenopausal osteoporosis. Drugs, calcium and vitamin D supplements and HRT can be used to treat the condition. Learn more about the other postmenopausal condition.